Diagnosing and treating pelvic pain
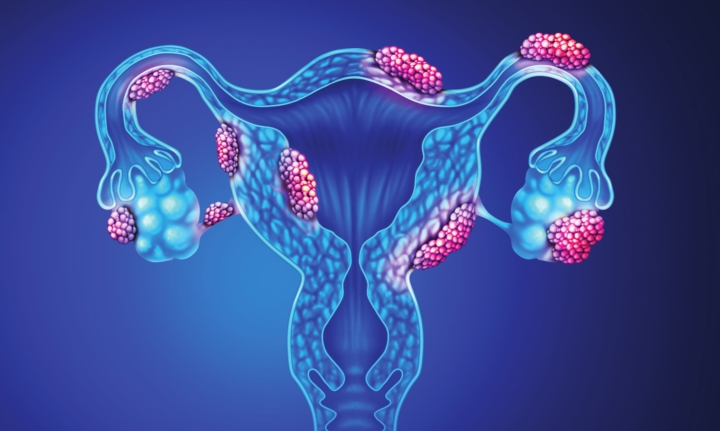
Endometriosis, a disease that causes tissue that normally lines the uterus to grow outside the uterus, affects approximately 8% of young women. It is commonly associated with pelvic pain that may also manifest as abdominal and back discomfort. Affected women may also have painful menstrual cycles, painful intercourse, difficulty conceiving children or infertility. In rare cases, endometriosis patients may report blood in urine, painful urination or painful bowel movements and bloody stools. Endometriosis is driven mainly by estrogen, which fuels the production of inflammatory agents that result in pelvic adhesions and pain. This results in some organs sticking to one another in the abdomen or pelvis.
According to one of the many theories,
endometriosis may happen when cells and tissue from the inner lining of
the uterus bleed “backwards” through the Fallopian tubes into the
pelvis during menstruation. Once there, the cells and tissue may implant
on the adjacent organs, including tubes, ovaries, uterus and other
associated structures. When on the ovaries, the cells and tissues can
also develop into cysts that fill with thick, dark material, commonly
called chocolate cysts, or formally named endometriomas. This tissue
often causes cyclical pain.
Endometriosis
is not so easy to diagnose. When patients have cyclic pain that seems
to worsen over time or discomfort with intercourse, they may need to be
evaluated by their OB/GYN doctor. The practitioner will perform a
vaginal exam and may order tests, such as a transvaginal ultrasound.
Sometimes direct visualization may be needed for diagnosis with what is
known as laparoscopy. In laparoscopy, a small incision is made near the
belly button, and a camera is inserted into the abdomen and pelvis to
visualize the endometriosis implants if present. However, not all
endometriosis implants are easy to identify or visualize.
The
first line of treatment for en dometriosis includes anti-inflammatory
medications, such as Ibuprofen, Naproxen, Diclofenac and others. Some
doctors may suggest birth control pills or progesterone supplementation,
which may be taken by mouth, injections, intrauterine devices or
underthe-skin implants. Other treatments do exist. When there is no
response to the above and fertility is not an issue, cycles can be
interrupted with continuous birth control pills or a hormone called GnRH
to help address the pain.
However,
GnRH does lead to signs of menopause and can also cause the weakening
of the bones if used longterm. Surgery is considered when these
additional medical treatment options are unsuccessful, and there are
masses to remove. Although this procedure may help, recurrence of the
pain is still possible. Hysterectomy may be considered for those who do
not plan to have children as it may specifically help with painful
periods, excessive bleeding and pain with intercourse.
Researchers
believe that endometriosis affects over six million women in the United
States. As physicians and surgeons, OB/GYN practitioners develop a
multitude of empathy for patients with endometriosis. If you are
experiencing symptoms or have concerns about your reproductive health,
please see a health-care professional, as many great treatment choices
are available.
Nasreldin M. Ibrahim, Ph.D., M.D, FACOG, is an assistant professor of OB/GYN at LSU Health Shreveport.