Possible treatment options
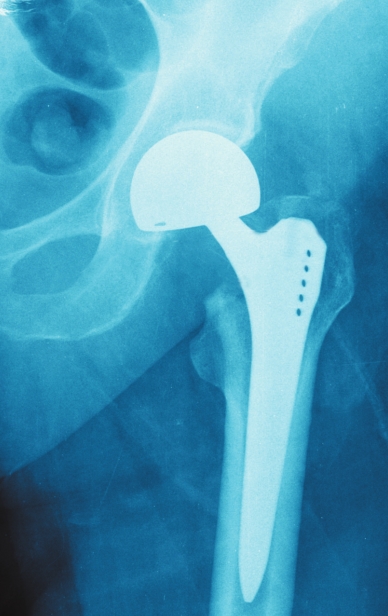
Total hip replacement surgery is extremely common, with more than 300,000 total hip replacements being performed in the United States annually. A total hip replacement procedure can be performed using a variety of surgical approaches, but the posterior approach, direct lateral approach, and direct anterior approach are by far the most common across the globe. Traditionally, most hip replacements have been done utilizing the posterior approach and direct lateral approach, where the surgeon accesses the hip through the side or buttocks. More recently, the anterior approach, where the surgeon enters from the front of the hip, has increased in popularity. The different approaches and whether one approach is better or produces a more optimal outcome have come under some debate. Does it matter if the surgeon enters either from the front of the body (anterior) versus the side/back (posterior) in a total hip replacement? Does one approach lead to a better outcome or faster recovery time? According to recent studies, the answer is no. The surgical approach to total hip replacement (THR) has no impact on outcomes six months following surgery. There is no difference if the surgical approach is to go from the front of the body (anterior) or the side/back (posterior).
This study conducted at Saint Francis Hospital & Medical Center in Hartford, Conn., involved 274 patients, who underwent THR between June 2012 and August 2014. Patients had THR with a surgeon either exclusively performing direct anterior approach or exclusively performing a posterior approach. The two groups were compared on the following: pre-/post-operative pain, function in daily living, function in sports and recreation, and hip-related quality of life. This study was presented at the annual meeting of the American Academy of Orthopedic Surgeons in March of 2016. Numerous other studies have been conducted and ultimately have come to the same conclusion.
Some claims and marketing campaigns have been made
that the direct anterior or direct superior approach are “minimally
invasive,” “no muscle cut” and “rapid recovery.” Realistically, there is
no clinical data to support these claims. It’s not the surgical
approach your surgeon utilizes; it’s your surgeon’s experience with that
surgical technique. I have patients who will come in to to see me and
will ask if I utilize “minimally invasive techniques.” This is simply
not a phrase that most orthopedic surgeons embrace. In my opinion,
undergoing hip replacement does not fall into the “minimally invasive”
category, and that is true no matter what surgical approach I utilize. I
am glad that patients have more resources to research the available
techniques for hip replacement. The well-versed patient is often better
prepared to start a conversation with their surgeon, and if you learn
that you are a candidate for total hip replacement, the initial dialogue
between the patient and surgeon is critical. At this point, it is
important that the patient learns which approach the surgeon is most
comfortable performing, which approach is most suitable for the patient
and set realistic preoperative goals and expectations for the surgery.
I
currently utilize two approaches: anterior (front of the hip) and
direct lateral approach (side). When utilizing the direct lateral
approach, I also utilize the Mako Robotic System, which combines the use
of a patient’s CT scan to create a customized surgical plan before the
surgery. In the OR, I guide a
robotic arm to follow your customized surgical plan created
preoperatively. When I utilize the anterior approach, I do have certain
criteria and guidelines that the patient must meet including current
health, height and weight restrictions.
It’s
important for patients to realize that they are the key player in
achieving a healthy outcome. Opening the line of communication with your
surgeon is essential. You must determine realistic goals and
expectations from the moment you have decided to have surgery. Do your
research, ask the questions and do the work.
Once
I have scheduled a patient for total hip replacement, and we have
determined the healthiest surgical approach to utilize, I give them a
hip-strengthening and exercise guide that I want them to begin working
on before surgery. This strengthening and exercise guide will also be
utilized following their surgery, as well. Most patients undergoing hip
replacement will spend one to two nights in the hospital and will be
able to return home. While in the hospital, they will work with a
physical therapist and be sent home with exercises and walking program
to follow postoperatively. I encourage patients to go to outpatient
therapy if they can. Outpatient physical therapy following hip
replacement can address common issues following hip replacement such as
irregular gait.
I
have had patients whose hip pain has caused them to rely on
wheelchairs. This affects their quality of life drastically. Following
their surgeries, they have been able to get out of their wheelchairs and
have progressed quickly to a walker or cane. When I see these patients
for their follow-up visit a couple of weeks after surgery, and they are
moving and feeling so much better, I realize this is why I do what I do!
If you have hip pain and it is affecting your quality of life, I
encourage you to visit with your family doctor or orthopedist. Start the
conversation and learn about all your options – surgical and
non-surgical.
Chase
Lobrano, MD, is a fellowship-trained orthopedic surgeon specializing in
total joint replacement of the knee and hip. Dr. Lobrano practices at
Orthopedic Specialists of Louisiana and Specialists Hospital Shreveport.